Welcome to ACT Playgroups
ACT Playgroups is a passionate non-profit community organisation that supports all playgroups and the benefits
which playgroups provide for families with young children across Australian Capital Territory.
THANK YOU
Your support is always appreciated!
ACT Playgroups delivers a range of events throughout the year. These range from Come and Try Playgroups in the school holidays to World’s Biggest Playgroup and Playfest.
Find out what’s coming up next.
Parent Testimonials
“Informative, empowering and encouraging.”
“Early Support Playgroup gives me an outlet. Coming to this Playgroup is a highlight of our week. My daughter is happy and so am I.”
“Coming to playgroup has helped motivate me to be a stronger advocate for my son and has assisted to build resilience in me in order for this to happen”
“It was awesome and inspiring – Thank you!”
Our Latest News
Have a read of some of the wonderful stories and experiences from our Playgroups
…and some formal updates too!
Playgroup Support and Development Worker
ACT Playgroups is looking for an experienced and motivated person to help support our range...
Holiday Break
The ACT Playgroups team is taking a much-needed break and is busy planning a play...
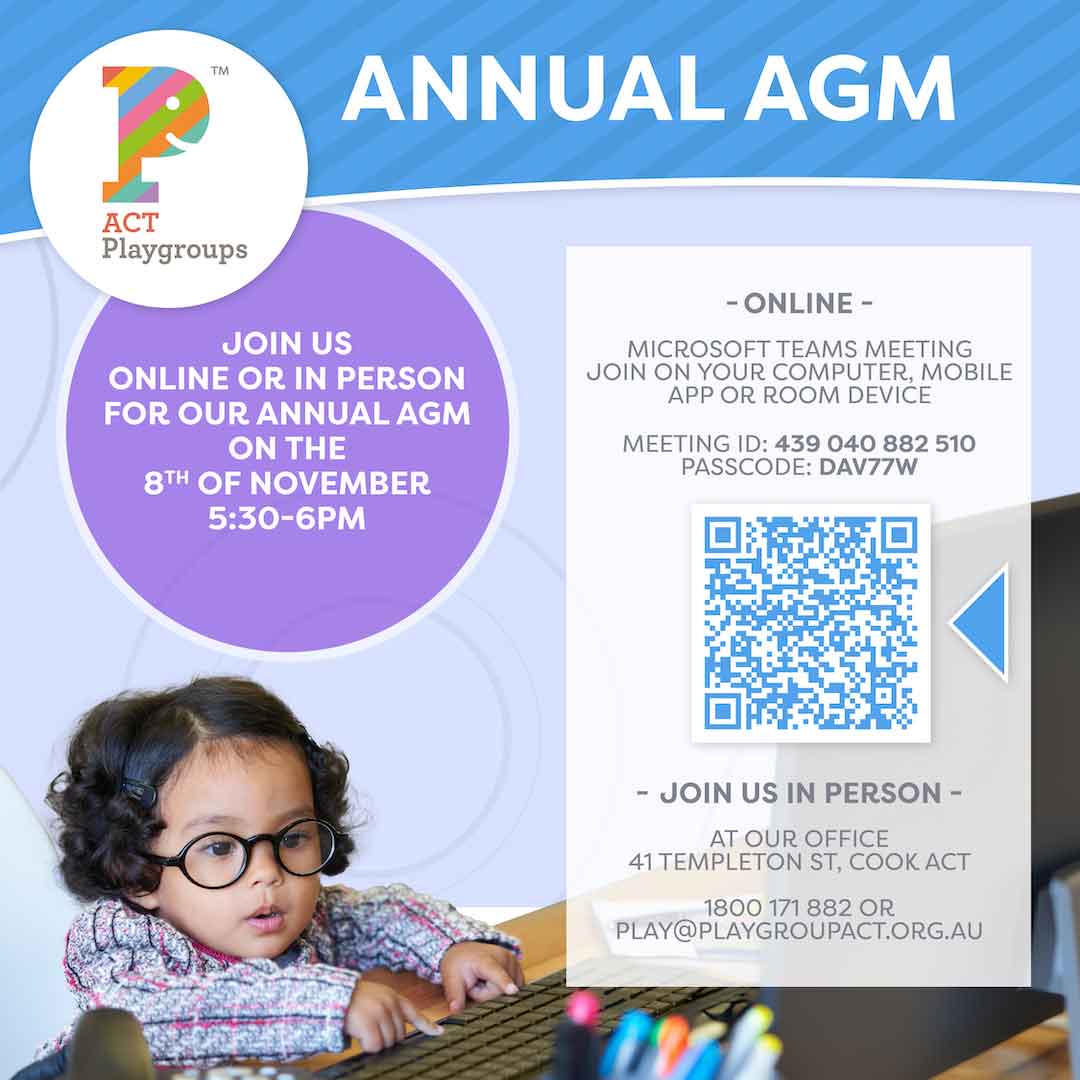
Annual AGM
You’re invited to attend ACT Playgroups AGM. Come along and hear all about the programs...